Share This Article:

Acute Low Back Pain: Be Careful what you Assume
Understanding Pain, Part 1
One of my physical therapy professors concluded a lecture by emphatically stating that the biggest piece of career advice he would impart was to never assume anything. As we exited the lecture hall, a classmate and I were skeptical, remarking that we found his comment to be, well, underwhelming. How could assumptions impact our careers?
'How Long 'til it Grows Back?'
Fast forward to a Saturday morning a few years later.
Working as a physical therapist, I was reviewing an orthopedic patient’s chart when, directly in front of me, two orthopedic surgeons exited a patient’s room – the patient I was there to evaluate. The surgeons collapsed into two chairs at the nurse’s station in obvious distress. The patient’s nurse hurried toward them and after a brief hushed exchange, all three were visibly agitated. Before continuing my chart review, I joined their conversation. The patient – a man in his early 20s – had sustained a severe injury in a workplace accident the day before and his lower leg would need to be amputated. The orthopedic surgeons delivered the news to the young man and his parents that the blood supply to the leg couldn’t be salvaged and there was no alternative.
The room was silent for a moment before the patient’s father calmly asked, "Doc, how long 'til it grows back?"
The orthopedists were stunned at this question. The patient encounter became much longer as the orthopedic surgeons explained that the lower leg wouldn’t grow back and outlined the sequence of planned medical treatment, fielding many more questions than they’d initially expected. The orthopedists and nurse were insistent -- there should be no assumptions with this patient or his parents.
More Info than Ever, More Need for Communication
We are living in remarkable times. Cutting-edge medical and research advancements, technological capabilities exceeding our wildest imaginings with near daily AI developments, influence from social media, and enormous access to resources. The internet, for example, offers more information than ever before. Yet, none of these advancements ensure that decisions are based on the most accurate or up-to-date information.
My physical therapy professor’s advice remains exceedingly relevant. Never assume anything.
Dialogue and communication are critical to uncover bias, judgments, misconceptions, and knowledge gaps. Pause to consider if the orthopedic surgeons hadn’t stayed in the patient’s room to discover the enormous misunderstanding of the planned surgery and its consequences? And yet, is this patient or medical encounter unique? How often are assumptions made that complicate claim management, negatively impact medical outcomes, or introduce legal challenges?
What do you Know about Low Back Pain?
Low back injury is one of the most prevalent workplace injuries, as well as one of the most common reasons for primary- and emergency-care consultations.1 It’s estimated that roughly 80% of adults will experience low back pain at some point in their lives and roughly one quarter of U.S. adults have back pain at any given time.2
Low back pain has multiple risk factors, including genetic profile, lifestyle factors such as increased body weight and smoking, physical factors such as poor posture and sedentary lifestyle, psychological factors such as stress, anxiety, and depression, comorbid conditions, and work-related factors such as heavy lifting, prolonged sitting, and physically demanding jobs.
Natural aging of the spine is a risk factor for back injury for which many, including the employees on the job and injured workers are largely unaware. The spine begins to age in the 20s and 30s, continuing a process of age-related deterioration throughout life. Vertebrae that compose the spinal column decrease in bone density and discs between the vertebrae gradually lose water content, becoming thinner and less flexible. Coupled with loss of core muscle strength as we age, an aging spine can become more stooped or curved.
Why is this Important?
Low back pain is one of the most prevalent medical conditions in worker’s compensation. Treatment of low back injury consumes a large percentage of workplace medical costs and can lead to costly and potentially unnecessary surgery. Add to this a provider’s plan for treatment and ability to potentially tease out patient-related misunderstandings or expectations for a return to "pain-free living," as well as myriad issues for the employer and payer.
All parties involved -- injured workers, providers, payers, employers, and courts and attorneys -- make decisions based on our educational and professional experiences, our personal experiences, and our own bias, judgments, and assumptions, many times without realizing what’s contributed to our thought process or decision-making. It’s not surprising that low back injury can be an overwhelming and thorny condition to manage and direct to a successful outcome.
What's to Come
Five additional articles will be presented in this series for each of the stakeholders in workers’ compensation: the injured worker, the provider(s), the employer, the payer, and potentially, the attorney. Despite unprecedented advancement in medical treatments, access to information or system improvements from artificial intelligence, successful outcomes require dialogue and communication to uncover bias, judgments, misconceptions, and knowledge gaps.
Are assumptions being made that are unknowingly derailing a claim and leading to dissatisfaction for an injured worker and potentially resulting in litigation? Or a poor surgical outcome? This series will examine how these factors contribute to a familiar topic in workers’ compensation.
Stay tuned!
References
- https://www.ncbi.nlm.nih.gov/books/NBK538173/
- https://pubmed.ncbi.nlm.nih.gov/17077742/
How can Evidence Beat Assumptions about Pain? Follow the Facts
Article 2 – Provider
A Weak Back?
When Marvin, a warehouse worker, tweaked his back lifting a box, the narrative began writing itself.
- The supervisor muttered, “He just doesn’t want to work.”
- The claims adjuster sighed, “Another soft-tissue claim? Expect six weeks of PT.”
- Marvin himself thought, “Maybe I’m just weak; my buddy was back in two days.”
- The physician at the occupational health clinic wondered, “This company has had so many back injuries. What’s wrong over there?”
Sound familiar? Assumptions, judgments and misconceptions can quickly take over this claim unless all parties are willing to dig deeper.
This series of articles posits that achieving successful outcomes following low back injury requires open dialogue and communication to surface biases, challenge assumptions, and address misconceptions or potential knowledge gaps.
All parties involved -- the injured worker, the provider(s), the payer, the employer, and potentially, the attorney -- make decisions based on educational and professional backgrounds, life experiences, as well as our own biases, judgments, and assumptions.
This second article in the series examines the healthcare provider. What judgments, assumptions, or knowledge gaps must be addressed by physicians, surgeons, physical therapists, nurse case managers, and other providers address to manage workplace low back injury?
Low Back Pain Medical Management Has Changed
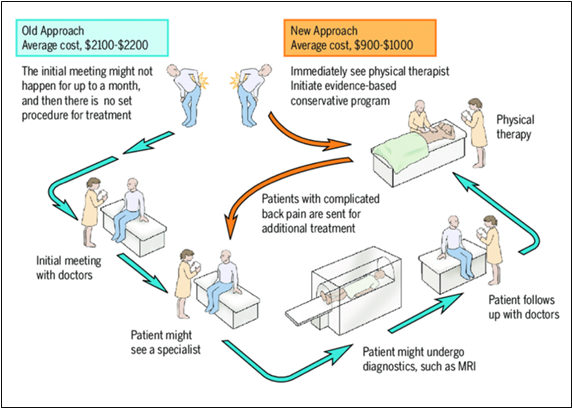
Traditionally, care for low back pain in the US was initiated with an appointment with a doctor, followed by an additional visit to a specialist; diagnostic testing, such as an MRI; a follow-up appointment with a doctor; and possibly referral to physical therapy.
Virginia Mason Medical Center piloted a program that directed patients with low back pain (LBP) immediately to see a physical therapist for an evidence-based conservative management approach. Patients with complicated LBP would be referred on for additional treatment or follow-up with their primary care provider after completing physical therapy.
Study results, published in 2011, reported a reduction of 23% in use of advanced imaging, 95% of patients received a same-day appointment, 91% of patients were satisfied with the process, and cost savings averaged $1,100 to $1,300 per patient.1 This clinical study and several others have been the catalyst for change in a movement toward evidence-based LBP management, reductions in imaging and other unnecessary interventions for non-specific low back pain, and early intervention to avoid delays in care, resulting in improved patient outcomes and cost savings.2-4
During the same that that new evidence-based pathways were changing low back pain management, the opioid epidemic was spiraling out of control. Overprescribing reached a climax in 2012 when health care providers wrote 259 million prescriptions for painkillers, roughly one for every American. 5 An overreliance on opioids as first-line treatment for low back pain has been replaced with a multi-modal approach that includes patient education for physical activity instead of rest as part of treatment, non-opioid medicines, lifestyle changes, stress management, early access to physical therapy, identifying muscle weakness, poor posture, and other root causes of back pain, and movement away from pharmacologic therapies, if possible. The goal of treatment has broadened to include not only pain reduction but also improving a patient's function and overall quality of life.
Changing a Patient’s Mindset
Physicians and clinicians must constantly revise their practice patterns as evidence-based approaches are introduced. Clinical and research data have prompted a growing awareness of the harm of unnecessary tests, treatments, and procedures, for example.6 Reshaping patients' perceptions and public awareness? That can be tricky. Dr. Doug Burton, a distinguished spine surgeon and Professor and Chair of the Department of Orthopedic Surgery at the University of Kansas Medical Center, acknowledges that patients assume they know what they need.
His approach?
"Explain the facts and the evidence. I prefer to have patients answer my questions instead of having them describe what they think is wrong. Navigate carefully, establish trust – without alienating. And tell them the painful truth, when necessary. If you take the time to explain it, they’ll accept it."
What Makes Low Back Pain a Thorny Issue?
Of all the workplace injuries, low back pain is in a class of its own. It’s the second most common reason for doctor visits and the leading cause of disability worldwide, including workplace disability.
"Low back pain wouldn’t be the #1 cause of disability if treatments worked well. Any time there’s widespread treatment options, it’s because none of them work very well," says Burton. "Only 60% of patients are considered to have a successful outcome after back fusion surgery. It’s the least successful operation in orthopedic surgery."
Low back surgery, including lumbar fusion surgery, is no stranger to workers’ compensation. Stakeholders – payers, claims adjusters, employers, supervisors, and healthcare providers - frequently shudder when fusion surgery enters the discussion for a workers’ compensation claim. Studies suggest that the U.S. performs lumbar fusions at a higher rate compared to many other developed nations.7 With so many factors at play – deterioration of the spine as we age, a host of treatment options, the need for providers to be judicious in selecting evidence-based treatment, the myriad risk factors that contribute to injury, it’s not surprising that low back pain treatment and management can be downright tricky.
Be Aware of Judgments
It’s human nature to make judgments and assumptions and yet most of us think we’re free from bias. Dr Burton’s perspective?
"A lot of people choose which side they’re going to take. Healthcare providers, physicians, surgeons, claims adjusters, bosses, and so on. We all make judgments to choose a side."
His suggestion for success in management of low back pain?
"The provider needs to choose the side of what is medically correct. This can be hard. You can appear to be pro patient or pro employer, but you ultimately need to follow the facts. Just like the TV show."
An old TV series, Dragnet, had an iconic tagline: Just the facts, ma’am. Dr. Burton recommends that same no-nonsense, fact-based approach for evaluation and treatment. Follow the facts when making decisions.
"Be honest. Surgeons can be conflicted by operating on people, so we need to check that. It’s hard to do, though. To be as good as you can, you need to be introspective. Identify your personal bias and put that away. It’s difficult to be brutally honest with yourself. Acknowledge your own fallibility. Look at yourself first if the patient is having a problem. Being truly honest with your patient will serve you better than anything else," Dr Burton says.
What happens to assumptions, judgement, and bias with this approach? They’re no longer a barrier. A new way forward is possible.
Expectation for Evidence-Based Care and its Ripple Effect
Despite advances in management of low back pain, the challenge remains to evaluate traditional models and habits. Medical services represent over 60% of the total cost of all workers’ compensation costs8 and the average medical cost per claim has had a threefold increase in the past 20 years.9
Recent studies have shown that physical therapy as a first-line treatment can reduce the overall cost of care, reducing long-term opioid use and lower likelihood for advanced imaging.10 Recent clinical practice guidelines for low back pain reexamine the traditional approach for physical therapy visits for a set number of visits per week in favor of an individualized approach, tailored to each patient’s needs and response to treatment.
There’s a growing understanding of the need for patients to be actively engaged in a home program for long-term management. Motivational interviewing, taking advantage of a few extra minutes during a patient encounter to identify other contributory factors (stress, anxiety, financial concerns, for example) can be impactful. Low back pain is a subjective experience caused by a host of factors, so providers are continually encouraged to engage with patients to identify the underlying contributors to their pain and guide them toward appropriate treatment.
Primary care is already facing a serious provider shortage, and projections indicate the trend will continue to worsen. In some states and for some workers’ compensation systems, physical therapists can act as primary treating providers, especially for musculoskeletal injuries. Even with supportive legislation in some states, some healthcare providers may be hesitant, as this shift challenges their familiar ways of working and underlying assumptions. There are a host of other innovations in management of low back injury care – use of AI to guide clinical decision-making and track outcomes, sharing outcome metrics with patients, providers, and payers for shared decision-making. Success for providers requires challenging long-held beliefs and entrenched practice patterns.
Summary
And Marvin, who tweaked his back at the warehouse? Rather than fitting this case into a template, the healthcare team dug deeper:
- The occupational health physician ruled out red flags.
- The physical therapist explained to Marvin how individual recovery isn’t one-size-fits-all. Physical therapy documentation included clear guidelines for modified duty so Marvin could return to work during his recovery.
Could the other stakeholders close gaps to contribute to an ideal outcome?
- The employer can educate the supervisor that early, active care—not rest or blame—improves outcomes.
- The underwriting team can flag this claim, prompting the payer and employer to coordinate a plan for an onsite physical therapist to perform job site analysis, ergonomic assessment, and even pre-employment screenings to identify risk factors for low back injury.
- The claims adjuster can be coached on function-focused metrics rather than timelines.
The result? Marvin would feel heard, engaged in his care, and safely return to modified work—proving that a weak back wasn’t the issue. It was assumptions and bias. Healthcare providers – physicians, surgeons, physical therapists, nurse case managers, and others – can play an influential role by "following the facts" to erase judgments and assumptions. A commitment to evidence-based practice in the evaluation, treatment, and management of workplace low back injury can be the difference.
The next article in the series will explore the injured worker’s perspective. More to come!
References
- Collaboration among providers, employers, and health plans to transform care cut costs and improved quality. Health Aff (Millwood). 2011;30(9):1680-1687. doi:10.1377/hlthaff.2011.0291
- Morgan T, Wu J, Ovchinikova L, et al. A national intervention to reduce imaging for low back pain by general practitioners: a retrospective economic program evaluation using Medicare Benefits Schedule data. BMC Health Serv Res. 2019;19:983. doi:10.1186/s12913-019-4773-y
- Morgan M, Shinost C, Mendez S, et al. The effect of early physical therapy intervention on case duration and physical therapy visits in acute work-related musculoskeletal injuries across body regions: a retrospective cohort study. JOSPT Open. 2025;3(3):333-353. doi:10.2519/josptopen.2025.0135
- Tucker M. Early PT for lower back pain sends fewer patients to specialists. Medscape. Published August 11, 2022. Accessed August 7, 2025. https://www.medscape.com/viewarticle/979089
- Murphy T. ICYMI: Murphy publishes op-ed on fentanyl epidemic. Published 2012. Accessed August 7, 2025. https://murphy.house.gov/media/press-releases/icymi-murphy-publishes-op-ed-fentanyl-epidemic
Centers for Disease Control and Prevention. CDC grand rounds: prescription drug overdoses—a U.S. epidemic. Published July 1, 2014. Accessed August 7, 2025. https://archive.cdc.gov/#/details?url=https://www.cdc.gov/media/releases/2014/p0701-opioid-painkiller.html - Born KB, Levinson W. Choosing Wisely campaigns globally: a shared approach to tackling the problem of overuse in healthcare. J Gen Fam Med. 2018;20(1):9-12. doi:10.1002/jgf2.225
- Cherkin DC, Deyo RA, Loeser JD, Bush T, Waddell G. An international comparison of back surgery rates. Spine. 1994;19(11):1201-1206.
- NCCI Holdings. Medical cost trends: then and now. WorkersCompensation.com. Published November 6, 2017. Accessed August 7, 2025. https://www.workerscompensation.com/news_read.php?id=27920
- NCCI Holdings. 2019 state of the line guide. NCCI.com. Published 2018. Accessed August 7, 2025. https://www.ncci.com/SecureDocuments/SOTL-Guides/SOTL_Guide_2019.pdf
- Childs JD, Fritz JM, Wu SS, et al. Implications of early and guideline-adherent physical therapy for low back pain on utilization and costs. BMC Health Serv Res. 2015;15:150. doi:10.1186/s12913-015-0830-3
Low Back Pain: The Injured Worker’s Perspective
Article 3
In clinical practice as a physical therapist, I quickly learned that there are many injuries and conditions that – following diagnosis - a patient learns about for the first time. A diagnosis of carpal tunnel syndrome, for example, requires an explanation of the relevant anatomy in the wrist and causal factors so the treatment plan and a home program can be understood. During the initial evaluation, a model of the body part or a colorful poster on the exam room wall can greatly aid this explanation.
This isn’t the case for low back injuries. If a patient hasn’t previously had a low back injury, a friend or family member has, and has passed along anecdotal accounts of the experience. Those stories, an internet search, comments from co-workers, or even comments from a healthcare provider, or a boss can shape an injured worker’s concept of low back injury and likely treatment.
This series of articles asserts that achieving a successful outcome following low back injury depends on open dialogue and communication to surface biases, challenge assumptions, and address misconceptions or knowledge gaps. All parties involved – the injured worker, the provider(s), the payer, the employer, and potentially, the attorney - make decisions based on education and professional background, life experiences, and potentially individual bias, judgments, and assumptions. This third article in the series will explore the injured worker’s perspective.
Age-Related Wear and Tear of the Spine
At roughly the time of entry into the workforce as adults, the spine shows evidence of aging, a process of gradual deterioration that continues throughout life. Bone density of vertebrae in the spinal column decreases and discs between those vertebrae slowly lose water content, becoming thinner and less flexible. As the spine and core muscles age, a curved or forward-facing posture may result. These age-related spinal changes may go unnoticed for those who are active and working.
Interpreting Imaging Results
For those unaware of natural aging of the spine, age-related findings on an X-ray or MRI can come as a complete surprise. A friend of mine in her late forties participated in a research study as a control group member and underwent MRI imaging of her lumbar spine. She was shocked that her imaging findings included lumbar disc degeneration, as well as a mild discal bulge, even in the absence of pain or symptoms. Her first thought upon reading the results was that she had mistakenly been given someone else’s imaging report!
This sense of bewilderment may sound familiar for healthcare providers, claims adjusters, and payers in workers’ compensation familiar with low back injury. Challenging the assumption that the spine is unaffected by age-related changes is a vital component of patient education. Without this context, interpreting abnormal findings can be exceedingly difficult.
There’s a straightforward connection between imaging results and the mechanism of injury for some body parts following a workplace injury. A carpal bone fracture reported on an x-ray seems logical after a fall onto an outstretched hand, for example. Imaging for the low back can be very different. Consider this injured worker’s interpretation of his imaging findings:
According to my MRI, there’s tons of stuff wrong with my back. And yet you’re trying to tell me that none of it is the result of my workplace injury?! I want to see a spine surgeon. I want all this fixed!
Incidental findings, which are unexpected abnormal findings unrelated to the reason the test was ordered, are increasingly common with the rise of advanced imaging techniques. When a workplace low back injury occurs, it can be difficult to separate degenerative spine conditions that are considered part of natural aging and not inherently compensable under workers’ compensation.
Work activities may accelerate but not cause abnormal imaging findings. Knowledge of imaging abnormalities can decrease self-perception of health and may lead to fear-avoidance and catastrophizing behaviors that may predispose an injured worker to chronicity.2 Patient education on interpreting imaging results, in particular, incidental findings, addresses knowledge gaps and misperceptions.
Catastrophizing Low Back Injury
Low back injury is a condition plagued with anecdotal misinterpretations and misinformation, so it’s not surprising that an injured worker may interpret the condition as far more negative than it is. Amy Garrett, PT, DPT, a physical therapist at Nebraska Spine & Pain Center and recognized expert in workplace injuries of the spine, says many patients are concerned about further injury, including catastrophic injury such as paralysis.
Dr. Garrett has found that education and explanation of the medical facts and evidence redirect fear of the worst possible outcome. To learn more about a patient’s concerns, she’ll ask, “And you are worried what could happen if you go back to work or do some exercises?”
Dr. Garrett handles fear, anxiety, and catastrophizing by asking additional follow-up questions regarding daily activities, such as who in the household is responsible for cooking, cleaning, laundry, and grocery shopping. She will connect daily tasks such as lifting a gallon of milk to lifting 8-10 pounds, for example. She recommends taking the time to make comparisons to work tasks and break down daily tasks that may be overwhelming into smaller, manageable parts. This approach identifies strategies for solutions and creates a plan of action to allay fears and personalize a treatment plan.
Healthcare Providers - Part of the Problem or Part of the Solution?
It’s important that physicians, surgeons, physical therapists, and nurse case managers consider the power of their words. Dr. Garrett says patients have told her, "My doctor says I have the spine of an 80-year-old’ or ‘It’s bone on bone’ or ‘If I keep doing this job, I could end up in a wheelchair.’" Comments such as these can be unsettling since they don’t draw a connection between the patient’s symptoms and recommended treatment, for example, or identify job tasks that may be contributing to a patient’s condition.
Emphasizing Patient Education
Traditional medical management of low back pain has undergone a significant shift to current evidence-based guidelines. Conservative treatments such as exercise, physical therapy, and lifestyle modifications are recommended as part of early intervention with medications and more invasive procedures reserved for cases where these initial steps aren’t sufficient. Although these guidelines have been in practice for more than a decade, there’s a sizable gap between best practices and common beliefs.
Many patients expect pain medication, including opioids as first-line treatment, imaging, injections, and possibly surgery. Because of this lack of public awareness, the World Health Organization (WHO) released its first-ever guidelines on managing chronic low back pain in 2023 to reshape unhelpful beliefs. WHO Guidelines include patient education on interventions, both recommended and not recommended, and suggestions for activities to promote good physical health, such as aerobic activity, strengthening, and flexibility exercises. 1
Reshaping Ideas on Rest and Recovery
Challenging the outdated belief that prolonged rest aids recovery after low back injury can be difficult. Dr. Garrett advises that providers get the patient moving again. Don’t assume they can lift or perform a particular task, though. Instead, help them gain the confidence they need to return to their life and their job.
The WHO Guidelines on low back pain state that delivery of care that is not evidence-based remains commonplace. Dr. Garrett is aware of this variation in care and the confusion it can create for injured workers. She recommends that passive modalities be avoided, especially after the first few weeks of injury.
"Get them moving. Get them on their feet squatting, doing sit to stands and doing functional movements in a pain free range to start giving them the confidence they need to do more."
One of the most common questions injured workers ask Dr. Garrett is “How much should I push it?” Dr. Garrett finds that she delivers a lot of education regarding the spine and nerve involvement, safe limits and restrictions on "pushing into pain" with the spine versus a knee or shoulder injury, injuries where pain may be expected to re-gain range of motion of the injured body part.
Summary
An injured worker’s concept of low back injury can be shaped by anecdotal experiences, comments from others, and misinformation. By recognizing the influence of potential assumptions, knowledge gaps and judgments, a successful outcome can be achieved through open dialogue and communication. All stakeholders – the injured worker, the provider(s), the payer, the employer, and potentially, the attorney - can challenge assumptions, and address misconceptions or knowledge gaps. The next article in the series will explore the employer.
Watch for more on this topic!
References
- World Health Organization. WHO guidelines on managing chronic low back pain. Published December 7, 2023. Accessed August 15, 2025. https://www.who.int/news/item/07-12-2023-who-releases-guidelines-on-chronic-low-back-pain
- Flynn TW, Smith B, Chou R. Appropriate use of diagnostic imaging in low back pain: a reminder that unnecessary imaging may do as much harm as good. J Orthop Sports Phys Ther. 2011;41(11):838-846. doi:10.2519/jospt.2011.3618
Same Video, Different Reports: How Assumptions about Pain Shape Observations
Article 4 – The Employer’s Perspective
There’s a classic learning activity used widely in schools and organizations in which a teacher or facilitator asks a group to watch a short video. Each attendee is then asked to describe aloud to the group what they saw. Even though everyone watched the same video, each person shares a different account. In fact, some observers may report a completely different version.
Why?
Each retelling is shaped not just by what someone saw, but by their own assumptions, fears, and life experiences. I participated in this activity during a graduate education class and found it to be quite startling. How could we see the same thing and yet have different reports? We don’t always see things as they are -- we see them as we are. Our assumptions, biases, and personal experiences color the ‘facts’ we think we’re reporting. The facts may be hidden beneath layers of perception and misperception.
Could this be occurring with workplace low back injury? I believe the answer is yes!
This series of articles asserts that achieving a successful outcome following low back injury depends on open dialogue and communication to surface biases, challenge assumptions, and address misconceptions or knowledge gaps. All parties involved -- the injured worker, the provider(s), the payer, the employer, and potentially, the attorney -- make decisions based on education and professional background, life experiences, and potentially individual bias, judgments, and assumptions. This fourth article in the series will explore the employer’s perspective.
Pre-Injury Assumptions Matter
An employee’s perspective and sense of connectedness at hire and in day-to-day culture matters. Creating a sense of connection and having open lines of communication between employees, supervisors, and company leadership are pivotal factors in an employee’s response to workplace injury. Research by the Workers Compensation Research Institute (WCRI) indicates that employees who fear losing their job or don’t understand the claims process following workplace injury are far more likely to seek legal representation.1
That fear typically arises from a lack of information and connection -- not from the severity of the injury itself. Waiting until an injury occurs to explain the workers’ compensation process or establish lines of communication isn’t wise. An employee in pain, under stress, and feeling isolated is more likely to misinterpret silence as indifference. A strategy by employers to address assumptions, fears, and bias early and often -- prior to a workplace low back injury -- is highly recommended.
Lifestyle Factors and Recognizing Warning Signs
Tom Slattery, CSP, ARM, is the Corporate Director of Safety for Norfolk Iron & Metal, one of the nation’s largest carbon, aluminum, and steel providers. With more than 30 years of experience in ergonomic assessment, risk management, and workers’ compensation, he’s aware that low back pain is one of the most prevalent medical conditions in worker’s compensation. He recognizes that many employees are unaware of the broad range of risk factors for low back injury and can mistakenly assume that physical workload factors are the sole contributor.
Age-related spinal changes and minor cumulative low back injury -- both in and outside of work -- are contributory. Lifestyle and modifiable factors such as eating and exercise habits, stress level, relationship and emotional demands, and financial pressures play a role in low back health and potential injury. Mr. Slattery recognizes that these knowledge gaps may cause an employee to miss warning signs that could have prevented injury. He regularly encourages early reporting to a manager or supervisor.
"Don’t wait until you’re on your knees in pain," Mr. Slattery advises. "Recognize the warning signs and speak up before an injury occurs."
Are Most Back Injuries the Result of Cumulative Trauma?
Mr. Slattery shared an analogy: "If an employee with years of cumulative trauma to the low back picks up a bath towel from the floor at home and that motion is sufficient to result in low back injury, the employee’s medical insurance plan covers the injury. However, if that same employee injures the low back by retrieving a pencil from the floor at work, it results in a workers’ compensation claim."
A common misperception he sees is that employees consider the "moment of injury" as solely causative instead of the cumulation of activities, movements and myriad other risk factors throughout their lifetimes which are contributory.
Put Away Judgment
When a low back injury occurs, Mr. Slattery encourages managers and supervisors to put aside judgments, bias, and assumptions.
"Questioning if the injury is legitimate or if an employee’s symptoms are real is a judgment that isn’t valuable," according to Mr. Slattery. Instead, he recommends focusing on the facts.
"The work we had them perform resulted in an injury," Mr. Slattery says. "Why wouldn’t we treat them well?"
Training for human resources teams and company supervisors encourages the mindset to "be that person. Be on their side."
Mr. Slattery points out that an injured worker home from work watching daytime TV will see commercials from attorneys planting doubt or fear, which can contribute to mistrust of the employer.
"If that happens, we didn’t do our job" Mr. Slattery says.
A physician who spoke at a workers’ compensation conference shared an analogy Mr. Slattery has never forgotten: "Visualize yourself handing an injured worker your credit card. Be personally invested in that employee’s care. It’s the moment of truth for your company and action is needed."
Communication as a Formula for Success
What does winning communication look like?
Dr. Amy Garrett, PT, DPT, physical therapist at Nebraska Spine & Pain and recognized expert in spinal workplace injuries says, "The more communication between all parties seems to be the best. I’ve had several patients who would text or email their case manager, and it seems like approvals happened more quickly and there were fewer delays because the case manager was more aware of what was happening with the case."
Mr. Brad Brons, a seasoned claims adjuster licensed in nine states with an exceptional understanding of anatomy and medical conditions/injuries, shares similar advice.
"During the initial phone call with an injured worker, I go out of my way to explain the claims process. I encourage them to call me after every visit with a healthcare provider so we can discuss what happened and what the plan is," Mr. Brons advises.
This has a two-fold benefit -- it sets up an opportunity to answer questions, explain any medical jargon the injured worker may not understand, and discuss "next steps" in evaluation and/or treatment. Since Mr. Brons also manages authorizations as part of his claims handling duties, it speeds up the process since he knows to watch for a referral or orders from an evaluating or treating physician.
Consider Your Audience
Mr. Slattery says an unfortunate assumption is to speak above an injured workers’ level of education.
Communication from claims adjusters or third-party administrators, for example, shouldn’t use industry-specific language in a formal letter that is beyond the 5th grade level. Terms specific to workers’ compensation that aren’t defined and offer little to no explanation for "next steps" in the process create confusion.
He recalled a claim in which an injured worker bemoaned, "The claims adjuster used words I didn’t understand. I’m not even sure when I’ll get paid."
Modified Duty with an Individualized Approach
Despite a common misconception that prolonged rest heals low back injury, it’s valuable to return an employee to work – as soon as possible – for a variety of reasons. Mr. Slattery reports that returning to work – modified duty, if necessary – maintains comradery with co-workers, contributes to a sense of control, and supports emotional well-being.
Dr. Garrett shares this view.
"It always seems to go better for the patient and the employer if there is some light duty or sedentary duty for the patient to participate in," according to Dr. Garrett.
Mr. Slattery points out that a mistake many companies make is not allowing any days away from work following low back injury.
"Sometimes, a day or two of rest isn’t always a bad thing," he recommends. "Be individualized in your approach.’
Mr. Slattery recalled that when he previously worked for an insurance company as an underwriter, a prospective company wouldn’t be offered a quote if they wouldn’t offer light duty after injury because "it’s that important."
Summary
And the short video shown as part of a learning activity in classrooms and organizations?
Assumptions, biases, and personal experiences may lead viewers to color the "facts" that are reported, potentially resulting in accounts that are completely different. Similarly, layers of perception and misperception exist for all parties involved in workplace low back injury – the injured worker, the provider(s), the payer, the employer, and potentially, the attorney.
Consideration for pre-injury assumptions, judgments by employers and supervisors, frequent communication at an appropriate level, and an individualized approach for return to work can contribute to a successful outcome for employers managing low back injury. The payer’s perspective will be considered in the next article in the series.
Stay tuned!
References
- Workers Compensation Research Institute. Avoiding Litigation: What Can Employers, Insurers, and State Workers’ Compensation Agencies Do? WCRI Report WC-10-18. July 2010.
How can ‘Financial First Responders’ Change Assumptions on Low Back Pain?
Article 5 – The Payer
Ever asked a stranger or new acquaintance what they do for a living only to receive a clever substitute instead of a direct answer? An interventional cardiologist I know tells folks that he’s in the plumbing business. A friend of mine who is an attorney tells others that he "argues for a living." I overheard a barista at a coffee shop identify himself to a customer as the "head grounds keeper." Using a clever substitute when asked your job title offers a humorous way to challenge someone’s initial judgments or bias. An insurance executive started a webinar I attended by saying that he was in the business of "taking people’s money to manage problems they hope will never happen."
For an industry that has recently come under much criticism, the clever substitute was likely delivered to set a positive tone for the rest of his remarks. As a "financial first responder," insurers or payers are called to serve and support when problems arise.
This series of articles asserts that achieving a successful outcome following workplace low back injury depends on open dialogue and communication to surface biases, challenge assumptions, and address misconceptions or knowledge gaps. All parties involved -- the injured worker, the provider(s), the payer, the employer, and potentially, the attorney -- make decisions based on their own experiences, which may include individual bias, judgments, and assumptions. This fifth article in the series will explore the payer’s perspective.
Let’s Just Get Right to It …
It’s the 500-pound elephant on the table -- the assumption that all workers’ compensation insurance companies question the legitimacy of an injury. It’s a stereotypical judgment that claims adjusters automatically assume not all injuries are genuine. And yet, isn’t it wise to trust, but verify? Challenging assumptions after a workplace low back injury requires lining up the facts.
After injury, the first aspect of patient evaluation is to gather information -- the injured worker’s symptoms, mechanism of injury or causative factors -- and perform an examination to determine a diagnosis. Based upon these initial findings, imaging or further tests may be ordered.
Dr. Doug Burton, MD, an accomplished spine surgeon and Professor and Chair of the Department of Orthopedic Surgery at the University of Kansas Medical Center, is aware of this common assumption.
"A lot of people choose which side they’re going to take. Healthcare providers, physicians, surgeons, claims adjusters, bosses, and so on," Dr. Burton says. "We all make judgments to choose a side."
Exam findings and medical records from the provider play a large role in determining compensability of a workplace injury, documenting its severity, and establishing the necessity of treatment. Brad Brons, a highly skilled claims adjuster who is licensed in 9 states, faces this frequently.
"I regularly assume I’m going to be seen as the bad guy," according to Brons. "There’s a mistrust of insurance companies in general. I know there are cases where that’s true, but I don’t see it with my company."
How Should Assumptions and Judgments be Managed?
Doing what’s right requires gathering evidence and assembling the facts. The due diligence by a workers’ compensation claims adjuster to interview the injured worker, the employer, the medical provider and review medical records is a necessary step. In doing so, it challenges assumptions and identifies inconsistencies, if they exist.
If concerns arise as the claim progresses, additional investigation may be needed. This may be carried out through surveillance, social media investigation, or medical canvassing to review an injured workers’ medical background and records. These measures may expose details that a claim has been inflated, is fraudulent, or is the result of a pre-existing condition.
Finger-Pointing Won’t Catch Fraud — Facts Will
Examining the payer perspective wouldn’t be complete without addressing the issue of workers’ compensation fraud. Previous reports have estimated that 1-2% of workplace injury claims are fraudulent.1 Fraud has typically been classified by the offending parties: premium fraud (employers) and claimant fraud (employees). And yet, every player -- the injured worker, the provider, the employer, the payer, and the attorney -- can commit fraud.
The Coalition Against Insurance Fraud formed its first-ever Task Force in 2021 to examine the topic of workers’ compensation fraud in the U.S.2 The Task Force set out to re-examine and update the long-standing $7 Billion estimate of workers’ compensation fraud annually in the US. Their investigation determined that the amount is roughly five times greater -- approximately $34 billion, $25 billion from employer fraud and $9 billion as the result of employee fraud.
A report published earlier this year by Conning, 2025 Workers' Comp Study: Using Data & AI to Fight Workers’ Compensation Insurance Fraud, estimates that workers’ compensation fraud costs insurers between $35 to $44 billion annually.3 By leveraging data and artificial intelligence (AI), insurers can proactively identify and combat fraudulent activities that have become increasingly sophisticated. Those who suggest fraud in workers’ compensation is uncommon or of little impact may need to address their own misconceptions and knowledge gaps.
On The Matter of IME’s
In the event of an injury for which surgery is recommended, it’s standard practice to seek a second opinion from another surgeon before proceeding. Conferring with another health care provider or surgeon affords us professional advice that we deem to be free from bias, allowing us to be confident that we’ve made the best decision.
Makes perfect sense, right?
An independent medical examination (IME) is intended to be an objective assessment of an injured worker’s medical condition, including the treatment needed, whether there’s a permanent impairment and to what degree, and the ability to work in the future. And yet, many injured workers view an insurance company’s request for an independent medical examination (IME) as unwelcome and unnecessary. It’s this unbiased perspective that Brad Brons finds extremely valuable if all the pieces don’t line up on a claim.
"IMEs can be wonderful," he says. "And if the case goes before a judge, most judges will recognize when a doctor is biased. Judges have seen it. They’ve worked as defense or corporate attorneys before becoming judges. That experience is huge."
Mr. Brons has been in the industry long enough to know that some medical decisions should be questioned and sees himself as an ally for his claimants. And if an IME report contradicts the injured workers’ treating physician? Mr. Brons doesn’t hesitate to recommend, "Trust the facts."
Does the Evidence Support an Injured Worker’s Mindset?
Low back injury can be a complex condition with multiple risk factors, causes, and treatment options that don’t always have successful outcomes. Although multiple factors may be contributory, Tom Slattery, CSP, ARM, Corporate Director of Safety for Norfolk Iron & Metal, points out "it’s that ‘moment of injury’ that many employees identify as causative. An employee may have a physically demanding job but also do physically demanding things at another job or as part of hobbies or family life and yet conclude that this job was to blame for the low back injury."
The initial phone contact that a claims adjuster makes to an injured worker includes questions that may potentially reveal if strenuous activity outside of work contributed to or was causative in low back injury. For injuries without an easily identifiable mechanism of injury such as cumulative trauma, it may be a difficult to challenge an injured worker’s assumptions.
Mr. Brons recognizes this after years of experience as a claims adjuster.
"People have an idea where the injury came from," according to Mr. Brons. "When that’s not validated, they get upset."
Our own stories provide the rationale for what’s happening. They’re our interpretation of the facts. By assembling the facts, feelings, emotions, and stories can be tested. Mr. Brons is familiar with age-related spine deterioration, the high degree of likelihood for incidental findings on low back imaging, and other factors that contribute to the complexity of low back injury. For an injured worker who isn’t knowledgeable of these issues, it can be downright frustrating.
Mr. Bron’s strategy to address this?
His above-average understanding of anatomy and medical conditions and perceptivity are critical to educate and answer questions during conversations with injured workers. Mr. Brons is grateful when providers -- spine surgeons, physicians, physical therapists -- explain the facts and the evidence.
"Some providers don’t have a good bedside manner and lack the willingness to educate," Mr. Brons advises. That’s when things break down."
If an injured worker isn’t given the opportunity to separate the facts from their story, it’s easy to see how resentment and frustration can result.
The Power of Communication and Consistency
Returning to work after following low back injury requires communication and coordination. It’s ideal when an insurer and employer share a similar vision to promote return to work strategies and overcome obstacles that might prevent this.
Amy Garrett, PT, DPT, an expert in workplace low back injury at Nebraska Spine & Pain says, "Assumptions without information are not usually helpful, so it’s best when a case manager or adjuster in coordination with the injured worker and the employer are working together to return the injured worker to meaningful work. Returning an injured worker to light duty, for example, can be so helpful to allow the worker to return to their typical work routine, allow them to socialize with their fellow workers, and move to participate in ADLs that they otherwise may not be doing at home. Frustrations often arise and significantly escalate if an injured worker is placed on light duty and then asked to do more than this by their employer."
Getting Back to Work – No Pun Intended!
Insurers in workers’ compensation must ensure that all parties are operating in the best interest of the injured worker. The treating physician or physical therapist, for example, has an expectation that the injured worker will be compliant with a home program and mindful of lifting restrictions or activity limitations, for example. The provider is responsible to safeguard and protect the worker from potential harm.
Amy Garrett, PT, DPT, points out, "I have seen other healthcare providers assume a certain level of strength in an injured worker which may not be accurate. Just because someone worked in a heavy or medium job does not mean that they don’t have flexibility or core strength deficits that need to be addressed. Building a strong foundation via exercise is vitally important, even with someone who has worked in a physically demanding job."
Summary
As a "financial first responder," insurers or payers are called to serve and support when problems arise. Regardless of the job title, all players involved -- the injured worker, the provider, the employer, the payer, and potentially, the attorney -- can unknowingly fall victim to assumptions, judgment and bias in workplace low back injury. Although these misperceptions may be deeply established, it’s possible to wade through a potentially challenging landscape armed with facts and evidence. Start by gathering medical facts after workplace low back injury, identifying inconsistencies, if they exist, gathering additional information through investigation or an IME, and communicating and coordinating with all parties to validate that a plan for return to work is safe and well executed.
This series of articles concludes with the final article examining the attorney’s perspective. Stay informed!
References
- Leigh JP, Markowitz SB, Fahs M, Landrigan PJ. Costs of Occupational Injuries and Illnesses. Ann Arbor, MI: University of Michigan Press; 2000. doi:10.3998/mpub.16885
- Coalition Against Insurance Fraud. Workers’ Compensation Fraud Task Force Report. Washington, DC: Coalition Against Insurance Fraud; 2022. Accessed September 17, 2025. https://insurancefraud.org/wp-content/uploads/WorkersCompFraudAmerica.pdf
- Conning, Inc. 2025 Workers' Comp Study: Using Data & AI to Fight Workers’ Compensation Insurance Fraud. Hartford, CT: Conning, Inc.; 2025. Accessed September 17, 2025. https://www.conning.com/about-us/news/ir-pr---ai-workers-comp
Challenging Assumptions about Pain? It all Comes Down to Trust
Article 6 – The Attorney
Your organization thinks it has a leadership issue.
Sales have been lagging for the past two quarters.
The latest marketing promotion has fizzled without the dramatic impact that was expected.
What’s the common denominator?
Trust. WSJ bestselling author David Horsager believes that lack of trust is the biggest expense of any organization.
The only reason people follow a leader is trust. The only reason people buy is trust. The only way to amplify a marketing message is to increase trust in that message. After meeting David, reading two of his books, and taking his Trust Edge course through a leadership group I'm in, I must agree.
This series of articles asserts that achieving a successful outcome following workplace low back injury depends on open dialogue and communication to surface bias, challenge assumptions, and address misconceptions or knowledge gaps. Following a workplace injury, the injured worker, provider(s), payer, and employer must collaborate throughout the duration of the claim to ensure its successful resolution. For some claims, a fifth party - the attorney – is introduced. Is loss of trust a factor? The final article in this series will examine the assumptions, miscommunications, and judgments that often arise in litigated claims.
Seeds of Misinformation
Even before a low back injury occurs, seeds influencing bias and judgment may be planted. It’s become second nature for individuals to conduct quick internet searches to gather information and anticipate potential diagnoses based on their symptoms. Ironically, this search for answers can yield a great deal of misinformation. Employers and payers in workers’ compensation are aware that Search Engine Optimization (SEO), the practice that helps a website achieve a higher search priority, allow local applicant attorneys to prioritize their website on a search of typical workplace injuries such as ‘low back pain.’
Narrative on these websites is frequently written in such a way to suggest who is likely to blame for an injury. It may appeal to emotions without any factual basis. Marketing messages may play to an injured worker’s frustration or preconceptions. If this influence doesn’t occur prior to a workplace injury, it may play out after an injury. Tom Slattery, CSP, ARM, Corporate Director of Safety for Norfolk Iron & Metal, points out that an injured worker who is home from work watching daytime TV will see commercials from attorneys. Frequently, these commercials plant doubt or fear, which can contribute to mistrust of the employer.
"If that happens, we didn’t do our job" Mr. Slattery says.
Adding One More to the Mix
Despite the potential complexities of workplace low back injury, many claims are resolved satisfactorily by the injured worker, employer, and payer. Under what circumstances does this fifth party become involved? The fifth party – an attorney – may be added if the back injury is significant or the claims process is particularly complex. Family and next of kin may hire an attorney for a workplace low back injury with a fatal outcome to handle all communication and negotiation with the insurance company, for example. Many litigated claims, however, don’t fall into these categories.
Research by the Workers Compensation Research Institute (WCRI) indicates that employees who fear losing their job or don’t understand the claims process following workplace injury are far more likely to seek legal representation.1 Julio E. Martinez, Esq. is an accomplished defense attorney, managing partner with Gilson Daub in the San Clemente, CA office, and Board Member of Hispanic Insurance & Risk Management Association. Based on his experience, Mr. Martinez observes that a breakdown with any of the three parties supporting an injured worker often leads the employee to seek legal representation:
- The employer (boss or supervisor)
- The provider (referring physician, surgeon, or physical therapist)
- The payer (claims adjuster with an insurance company or third-party administrator)
Mr. Martinez has seen typical scenarios emerge from his professional experiences.
The Employer
Mr. Martinez says the most common assumption or misconception made by a boss or supervisor is that the injured worker isn’t telling the truth.
"When an employee reports an injury to a supervisor, they will many times make a judgment that the injured worker is malingering or exaggerating. I’ve heard it multiple times. The boss or supervisor will tell me, ‘That person was a horrible worker anyway.’ But the injury was witnessed, I’ll counter. What does the person’s job performance have to do with it? How is that judgment relevant?" Mr. Martinez says.
Mr. Martinez recognizes the power of judgment and its enormous potential impact.
"Empathy is necessary at the onset. It's hard, I realize. Humans instinctively want to question. But empathy is much more powerful. We’d have much less litigation if employers could recognize this," he says.
If a boss or supervisor doesn’t recognize these internal judgments and assumptions, the claim is on a rocky course before it’s even formally filed.
Another misstep Mr. Martinez sees is an employer who doesn’t follow lifting restrictions or activity limitations from the provider.
"A doctor’s professional judgment shouldn’t be overlooked," according to Mr. Martinez. "Asking an injured worker to perform job tasks that exceed the doctor’s advice is an easy target for litigation."
Amy Garrett, PT, DPT, physical therapist at Nebraska Spine & Pain and recognized expert in spinal workplace injuries, shares this same observation, "Being asked to work at a level higher than their work restriction is a common trigger for hiring an attorney. In fact, I see it a lot."
Dr. Doug Burton, MD, a nationally recognized spine surgeon and Professor & Chair of Orthopedic Surgery at the University of Kansas Medical Center, commented, "Usually by the time they see the attorney, the trust between the injured worker and employer is gone. This lessens the chance for a good medical outcome. After an injured worker has been out of work for 1 year, less than 1% will go back to work. Only 5% will go back to work if given support."
Dr. Garrett has encountered patients who've hired an attorney due to failings they’ve perceived in how their boss/employer is handling the claim.
"I think the biggest frustration is lack of communication," says Dr. Garrett. "It seems that sometimes the patient becomes a case manager, carrying information between the medical staff and their employer."
The Provider
Successfully managing the medical aspects of a workplace low back injury – making a diagnosis, ordering diagnostic tests, performing surgery, and coordinating treatment – isn’t the only task for a provider. Equally important is taking the time to explain, educate, and listen.
"This is someone’s job. Their livelihood. They’re counting on the doctor to offer an explanation," Mr. Martinez says.
Given that everyone’s case is unique, a healthcare provider has a unique responsibility to interpret the mechanism of injury, signs and symptoms, imaging results, or other medical findings for an injured worker.
"Take time to answer questions," Mr. Martinez urges.
Another issue Mr. Martinez has observed occurs when multiple body parts are injured. He recently handled an admitted claim that should have been rather straightforward.
"It was a witnessed fall that included a video of the incident. The main injury was to the back, but the wrist was also injured. I took a deposition for an injured worker who was visibly upset. This man was seen for a Qualified Medical Examination (QME). The doctor hadn’t included the wrist as an authorized body part. The report only mentioned injuries to the back. After this employee read the QME report, he hired an attorney. Didn’t the QME physician realize what would happen?" Mr. Martinez laments. "It’s not uncommon that other body parts are injured with a low back injury. Your reporting needs to be accurate."
Mr. Martinez says wistfully, "One of my goals – in addition to my daily work – is to share what I’ve learned with doctors. See your patient from the perspective of a claim. No one else has your medical expertise. Consider how important your role is. Your reporting needs to be accurate. It’s worthless otherwise. If you read that two body parts are accepted, but another body part is legitimately injured, put that in your report."
He recalls an injured worker sharing with him, "That body part was overlooked, so I hired an attorney." Even if the complaints are minimal and there’s no permanent disability, report your findings.
"Be complete," implores Mr. Martinez.
The Payer
There are several potential lapses in judgment or misunderstandings by a payer that may prompt an injured worker to hire an attorney.
"An easy one: lack of communication from the claims adjuster," Mr. Martinez says.
A close second?
"A denial from UR (utilization review). If an injured worker receives a formal letter indicating a UR denial, many times it’s assumed by the injured worker that medical care has ended or there’s no option for reconsideration," Mr. Martinez advises.
An injured worker is likely to make assumptions or draw inaccurate conclusions if there isn’t immediate communication from a claims adjuster or nurse case manager to explain next steps or alternatives.
Mr. Martinez identified several UR decisions that resulted in litigation based on his review of medical records.
"For one case, an MRI took 4 months to get approved. Why?" Mr. Martinez asks.
Are criteria for medical necessity of imaging written to leave no room for interpretation?
"If an AME or QME will ultimately approve that MRI, why introduce a four-month delay to medical treatment or add additional expense to the claim?" Mr. Martinez says.
Mr. Martinez shared an example of a claim handled well. He reviewed a California claim: a pro per settlement. The unrepresented injured worker had sustained an injury to the neck, and the claims adjuster asked the primary treating physician (PTP) to leave future medical care open. Surgery was discussed, but it wasn’t medically indicated at the present time, and it wasn’t prudent to add surgical expenses to the claim settlement. By leaving medical care open, the injured worker would have the option for a physical therapy session or two, if needed, or re-evaluation by the physician.
"Little things add up," Martinez says. "This recommendation from the claims adjuster put the claim on course to be settled in a timely manner without adding extra expense and resulted in a very satisfied employee."
Summary
Achieving a successful outcome following workplace low back injury depends on open dialogue and communication to surface biases, challenge assumptions, and address misconceptions or knowledge gaps. This series of articles has examined the perspective of each of the parties involved – the injured worker, the provider(s), the employer, the payer - and, for some claims, the attorney. When trust is broken or communication is ineffective or absent between the injured worker and the provider, employer, or payer, this fifth party is introduced. By addressing judgment, assumptions, and seeds of mistrust, the provider(s), employer, and payer can navigate potential roadblocks for a favorable result.
References
- Workers Compensation Research Institute. Avoiding Litigation: What Can Employers, Insurers, and State Workers’ Compensation Agencies Do? WCRI Report WC-10-18. July 2010.
AI california case file caselaw case management case management focus claims compensability compliance compliance corner courts covid do you know the rule employers exclusive remedy florida glossary check Healthcare hr homeroom insurance insurers iowa leadership NCCI new jersey new york ohio pennsylvania roadmap Safety safety at work state info tech technology texas violence WDYT west virginia what do you think women's history women's history month workers' comp 101 workers' recovery Workplace Safety Workplace Violence
Read Also
About The Author
About The Author
- Anne Stanco
More by This Author
Read More
- Feb 19, 2026
- NCCI
- Feb 16, 2026
- Dennis Sponer
- Feb 14, 2026
- Amanda Conley Lauren Meadows
- Feb 13, 2026
- NCCI
- Feb 09, 2026
- Dennis Sponer
- Feb 05, 2026
- Michelle Despres




