Share This Article:

By AM Stanco
Article 2 – Provider
A Weak Back?
When Marvin, a warehouse worker, tweaked his back lifting a box, the narrative began writing itself.
- The supervisor muttered, “He just doesn’t want to work.”
- The claims adjuster sighed, “Another soft-tissue claim? Expect six weeks of PT.”
- Marvin himself thought, “Maybe I’m just weak; my buddy was back in two days.”
- The physician at the occupational health clinic wondered, “This company has had so many back injuries. What’s wrong over there?”
Sound familiar? Assumptions, judgments and misconceptions can quickly take over this claim unless all parties are willing to dig deeper.
This series of articles posits that achieving successful outcomes following low back injury requires open dialogue and communication to surface biases, challenge assumptions, and address misconceptions or potential knowledge gaps.
All parties involved -- the injured worker, the provider(s), the payer, the employer, and potentially, the attorney -- make decisions based on educational and professional backgrounds, life experiences, as well as our own biases, judgments, and assumptions.
This second article in the series examines the healthcare provider. What judgments, assumptions, or knowledge gaps must be addressed by physicians, surgeons, physical therapists, nurse case managers, and other providers address to manage workplace low back injury?
Low Back Pain Medical Management Has Changed
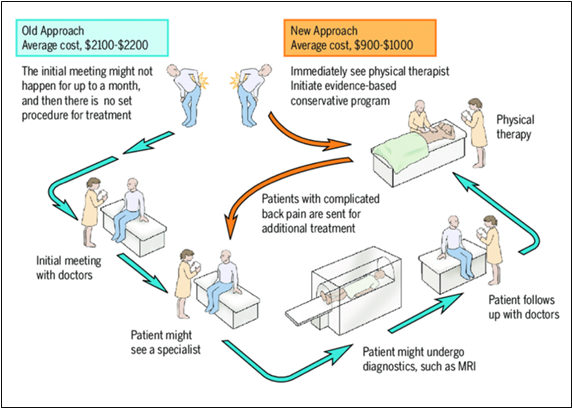
Traditionally, care for low back pain in the US was initiated with an appointment with a doctor, followed by an additional visit to a specialist; diagnostic testing, such as an MRI; a follow-up appointment with a doctor; and possibly referral to physical therapy.
Virginia Mason Medical Center piloted a program that directed patients with low back pain (LBP) immediately to see a physical therapist for an evidence-based conservative management approach. Patients with complicated LBP would be referred on for additional treatment or follow-up with their primary care provider after completing physical therapy.
Study results, published in 2011, reported a reduction of 23% in use of advanced imaging, 95% of patients received a same-day appointment, 91% of patients were satisfied with the process, and cost savings averaged $1,100 to $1,300 per patient.1 This clinical study and several others have been the catalyst for change in a movement toward evidence-based LBP management, reductions in imaging and other unnecessary interventions for non-specific low back pain, and early intervention to avoid delays in care, resulting in improved patient outcomes and cost savings.2-4
During the same that that new evidence-based pathways were changing low back pain management, the opioid epidemic was spiraling out of control. Overprescribing reached a climax in 2012 when health care providers wrote 259 million prescriptions for painkillers, roughly one for every American. 5 An overreliance on opioids as first-line treatment for low back pain has been replaced with a multi-modal approach that includes patient education for physical activity instead of rest as part of treatment, non-opioid medicines, lifestyle changes, stress management, early access to physical therapy, identifying muscle weakness, poor posture, and other root causes of back pain, and movement away from pharmacologic therapies, if possible. The goal of treatment has broadened to include not only pain reduction but also improving a patient's function and overall quality of life.
Changing a Patient’s Mindset
Physicians and clinicians must constantly revise their practice patterns as evidence-based approaches are introduced. Clinical and research data have prompted a growing awareness of the harm of unnecessary tests, treatments, and procedures, for example.6 Reshaping patients' perceptions and public awareness? That can be tricky. Dr. Doug Burton, a distinguished spine surgeon and Professor and Chair of the Department of Orthopedic Surgery at the University of Kansas Medical Center, acknowledges that patients assume they know what they need.
His approach?
"Explain the facts and the evidence. I prefer to have patients answer my questions instead of having them describe what they think is wrong. Navigate carefully, establish trust – without alienating. And tell them the painful truth, when necessary. If you take the time to explain it, they’ll accept it."
What Makes Low Back Pain a Thorny Issue?
Of all the workplace injuries, low back pain is in a class of its own. It’s the second most common reason for doctor visits and the leading cause of disability worldwide, including workplace disability.
"Low back pain wouldn’t be the #1 cause of disability if treatments worked well. Any time there’s widespread treatment options, it’s because none of them work very well," says Burton. "Only 60% of patients are considered to have a successful outcome after back fusion surgery. It’s the least successful operation in orthopedic surgery."
Low back surgery, including lumbar fusion surgery, is no stranger to workers’ compensation. Stakeholders – payers, claims adjusters, employers, supervisors, and healthcare providers - frequently shudder when fusion surgery enters the discussion for a workers’ compensation claim. Studies suggest that the U.S. performs lumbar fusions at a higher rate compared to many other developed nations.7 With so many factors at play – deterioration of the spine as we age, a host of treatment options, the need for providers to be judicious in selecting evidence-based treatment, the myriad risk factors that contribute to injury, it’s not surprising that low back pain treatment and management can be downright tricky.
Be Aware of Judgments
It’s human nature to make judgments and assumptions and yet most of us think we’re free from bias. Dr Burton’s perspective?
"A lot of people choose which side they’re going to take. Healthcare providers, physicians, surgeons, claims adjusters, bosses, and so on. We all make judgments to choose a side."
His suggestion for success in management of low back pain?
"The provider needs to choose the side of what is medically correct. This can be hard. You can appear to be pro patient or pro employer, but you ultimately need to follow the facts. Just like the TV show."
An old TV series, Dragnet, had an iconic tagline: Just the facts, ma’am. Dr. Burton recommends that same no-nonsense, fact-based approach for evaluation and treatment. Follow the facts when making decisions.
"Be honest. Surgeons can be conflicted by operating on people, so we need to check that. It’s hard to do, though. To be as good as you can, you need to be introspective. Identify your personal bias and put that away. It’s difficult to be brutally honest with yourself. Acknowledge your own fallibility. Look at yourself first if the patient is having a problem. Being truly honest with your patient will serve you better than anything else," Dr Burton says.
What happens to assumptions, judgement, and bias with this approach? They’re no longer a barrier. A new way forward is possible.
Expectation for Evidence-Based Care and its Ripple Effect
Despite advances in management of low back pain, the challenge remains to evaluate traditional models and habits. Medical services represent over 60% of the total cost of all workers’ compensation costs8 and the average medical cost per claim has had a threefold increase in the past 20 years.9
Recent studies have shown that physical therapy as a first-line treatment can reduce the overall cost of care, reducing long-term opioid use and lower likelihood for advanced imaging.10 Recent clinical practice guidelines for low back pain reexamine the traditional approach for physical therapy visits for a set number of visits per week in favor of an individualized approach, tailored to each patient’s needs and response to treatment.
There’s a growing understanding of the need for patients to be actively engaged in a home program for long-term management. Motivational interviewing, taking advantage of a few extra minutes during a patient encounter to identify other contributory factors (stress, anxiety, financial concerns, for example) can be impactful. Low back pain is a subjective experience caused by a host of factors, so providers are continually encouraged to engage with patients to identify the underlying contributors to their pain and guide them toward appropriate treatment.
Primary care is already facing a serious provider shortage, and projections indicate the trend will continue to worsen. In some states and for some workers’ compensation systems, physical therapists can act as primary treating providers, especially for musculoskeletal injuries. Even with supportive legislation in some states, some healthcare providers may be hesitant, as this shift challenges their familiar ways of working and underlying assumptions. There are a host of other innovations in management of low back injury care – use of AI to guide clinical decision-making and track outcomes, sharing outcome metrics with patients, providers, and payers for shared decision-making. Success for providers requires challenging long-held beliefs and entrenched practice patterns.
Summary
And Marvin, who tweaked his back at the warehouse? Rather than fitting this case into a template, the healthcare team dug deeper:
- The occupational health physician ruled out red flags.
- The physical therapist explained to Marvin how individual recovery isn’t one-size-fits-all. Physical therapy documentation included clear guidelines for modified duty so Marvin could return to work during his recovery.
Could the other stakeholders close gaps to contribute to an ideal outcome?
- The employer can educate the supervisor that early, active care—not rest or blame—improves outcomes.
- The underwriting team can flag this claim, prompting the payer and employer to coordinate a plan for an onsite physical therapist to perform job site analysis, ergonomic assessment, and even pre-employment screenings to identify risk factors for low back injury.
- The claims adjuster can be coached on function-focused metrics rather than timelines.
The result? Marvin would feel heard, engaged in his care, and safely return to modified work—proving that a weak back wasn’t the issue. It was assumptions and bias. Healthcare providers – physicians, surgeons, physical therapists, nurse case managers, and others – can play an influential role by "following the facts" to erase judgments and assumptions. A commitment to evidence-based practice in the evaluation, treatment, and management of workplace low back injury can be the difference.
The next article in the series will explore the injured worker’s perspective. More to come!
References
- Collaboration among providers, employers, and health plans to transform care cut costs and improved quality. Health Aff (Millwood). 2011;30(9):1680-1687. doi:10.1377/hlthaff.2011.0291
- Morgan T, Wu J, Ovchinikova L, et al. A national intervention to reduce imaging for low back pain by general practitioners: a retrospective economic program evaluation using Medicare Benefits Schedule data. BMC Health Serv Res. 2019;19:983. doi:10.1186/s12913-019-4773-y
- Morgan M, Shinost C, Mendez S, et al. The effect of early physical therapy intervention on case duration and physical therapy visits in acute work-related musculoskeletal injuries across body regions: a retrospective cohort study. JOSPT Open. 2025;3(3):333-353. doi:10.2519/josptopen.2025.0135
- Tucker M. Early PT for lower back pain sends fewer patients to specialists. Medscape. Published August 11, 2022. Accessed August 7, 2025. https://www.medscape.com/viewarticle/979089
- Murphy T. ICYMI: Murphy publishes op-ed on fentanyl epidemic. Published 2012. Accessed August 7, 2025. https://murphy.house.gov/media/press-releases/icymi-murphy-publishes-op-ed-fentanyl-epidemic
Centers for Disease Control and Prevention. CDC grand rounds: prescription drug overdoses—a U.S. epidemic. Published July 1, 2014. Accessed August 7, 2025. https://archive.cdc.gov/#/details?url=https://www.cdc.gov/media/releases/2014/p0701-opioid-painkiller.html
- Born KB, Levinson W. Choosing Wisely campaigns globally: a shared approach to tackling the problem of overuse in healthcare. J Gen Fam Med. 2018;20(1):9-12. doi:10.1002/jgf2.225
- Cherkin DC, Deyo RA, Loeser JD, Bush T, Waddell G. An international comparison of back surgery rates. Spine. 1994;19(11):1201-1206.
- NCCI Holdings. Medical cost trends: then and now. WorkersCompensation.com. Published November 6, 2017. Accessed August 7, 2025. https://www.workerscompensation.com/news_read.php?id=27920
- NCCI Holdings. 2019 state of the line guide. NCCI.com. Published 2018. Accessed August 7, 2025. https://www.ncci.com/SecureDocuments/SOTL-Guides/SOTL_Guide_2019.pdf
- Childs JD, Fritz JM, Wu SS, et al. Implications of early and guideline-adherent physical therapy for low back pain on utilization and costs. BMC Health Serv Res. 2015;15:150. doi:10.1186/s12913-015-0830-3
AI california case file caselaw case management case management focus claims compensability compliance compliance corner courts covid do you know the rule employers exclusive remedy florida glossary check Healthcare hr homeroom insurance insurers iowa leadership NCCI new jersey new york ohio pennsylvania roadmap Safety safety at work state info tech technology texas violence WDYT west virginia what do you think women's history women's history month workers' comp 101 workers' recovery Workplace Safety Workplace Violence
Read Also
About The Author
About The Author
- Anne Stanco
More by This Author
Read More
- Feb 19, 2026
- NCCI
- Feb 16, 2026
- Dennis Sponer
- Feb 14, 2026
- Amanda Conley Lauren Meadows
- Feb 13, 2026
- NCCI
- Feb 09, 2026
- Dennis Sponer
- Feb 05, 2026
- Michelle Despres




